MRD and Biomarkers
Establishing MRD Benchmark for Deployment of T-cell Redirection as Post Induction Therapy in Newly Diagnosed Multiple Myeloma
P-164: Establishing MRD Benchmark for Deployment of T-cell Redirection as Post Induction Therapy in Newly Diagnosed Multiple Myeloma
Thursday, September 26, 2024

Susan Bal, MD
Assistant Professor
University of Alabama at Birmingham, United States
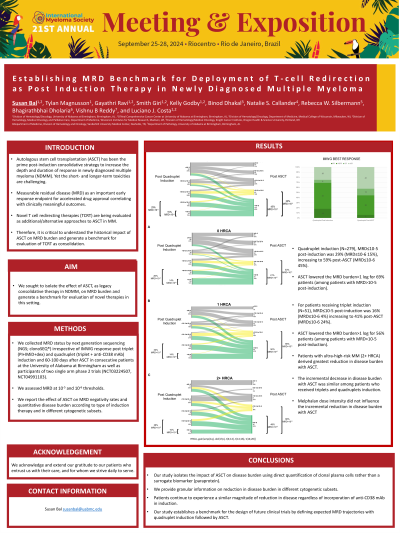
Introduction: Autologous stem cell transplantation (ASCT) has been the prime post-induction consolidative strategy to increase the depth and duration of response in newly diagnosed multiple myeloma (NDMM). The use of highly efficacious triplet and quadruplet induction regimens offering long term disease control have paved the way for minimal residual disease (MRD) as an important early response endpoint for accelerated drug approval correlating with clinically meaningful outcomes. Novel T cell redirecting therapies (TCRT) produce high response and MRD negativity rates in patients with relapsed MM, and numerous trials are underway to test their efficacy in early line treatment, including in NDMM as alternative to ASCT. Towards this end, it is critical to understand the historical impact of ASCT on MRD burden and generate a benchmark for evaluation of TCRT as consolidation.
Methods: We collected MRD status by next generation sequencing (NGS; clonoSEQ®) irrespective of IMWG response post triplet (PI+IMiD+dex) and quadruplet (triplet + anti-CD38 mAb) induction and 60-100 days after ASCT in consecutive patients at one large volume myeloma program along with participants of two single arm phase 2 trials with quadruplet induction followed by ASCT (NCT03224507, NCT04991103). We assessed MRD at 10-5 and 10-6 thresholds. We report the effect of ASCT on MRD negativity rates and quantitative disease burden according to type of induction therapy and in different cytogenetic subsets.
Results: We obtained post-induction and post-ASCT MRD in 330 patients, 124 (38%) were clinical trial participants, 279 (85%) had received quadruplet induction, 106 (33%) had 1 high-risk chromosome abnormality [HRCA, gain/amp(1q), del(17p), t(4;14), t(14;16), t(14;20)] and 44 (14%) had 2+ HRCA.
For patients receiving triplet induction, MRD≤10-5 post-induction was 16% (MRD≤10-6 4%) increasing to 41% post-ASCT (MRD≤10-6 24%). Among patients with MRD≥10-5 post-induction, ASCT lowered the MRD burden≥1 log for 56% patients.
For patients receiving quadruplet induction, MRD≤10-5 post-induction was 29% (MRD≤10-6 15%) increasing to 59% post-ASCT (MRD≤10-6 45%). When evaluating based on cytogenetic risk group among patients who received quadruplet induction, MRD< 10-5 post induction was 19%, 31% and 28% (MRD≤10-6 17%, 14%, 10%) which improved to 53%, 66% and 65% respectively, post-ASCT (MRD≤10-641%, 50%, 48%) of patients with 0, 1 and 2+ HRCA, respectively.
Among patients with MRD≥10-5 post-induction, ASCT lowered the MRD burden≥1 log for 69% patients (60%, 72% and 81% of patients with 0, 1 and 2+ HRCA, respectively).
Conclusions: This dataset provides granular data to delineate the impact of ASCT on MRD as legacy consolidative strategy in NDMM and provides an important benchmark for evaluation of efficacy of TCRT as experimental consolidative strategy. This information can guide effect size calculation in the design of ongoing and future TCRT trials.
Methods: We collected MRD status by next generation sequencing (NGS; clonoSEQ®) irrespective of IMWG response post triplet (PI+IMiD+dex) and quadruplet (triplet + anti-CD38 mAb) induction and 60-100 days after ASCT in consecutive patients at one large volume myeloma program along with participants of two single arm phase 2 trials with quadruplet induction followed by ASCT (NCT03224507, NCT04991103). We assessed MRD at 10-5 and 10-6 thresholds. We report the effect of ASCT on MRD negativity rates and quantitative disease burden according to type of induction therapy and in different cytogenetic subsets.
Results: We obtained post-induction and post-ASCT MRD in 330 patients, 124 (38%) were clinical trial participants, 279 (85%) had received quadruplet induction, 106 (33%) had 1 high-risk chromosome abnormality [HRCA, gain/amp(1q), del(17p), t(4;14), t(14;16), t(14;20)] and 44 (14%) had 2+ HRCA.
For patients receiving triplet induction, MRD≤10-5 post-induction was 16% (MRD≤10-6 4%) increasing to 41% post-ASCT (MRD≤10-6 24%). Among patients with MRD≥10-5 post-induction, ASCT lowered the MRD burden≥1 log for 56% patients.
For patients receiving quadruplet induction, MRD≤10-5 post-induction was 29% (MRD≤10-6 15%) increasing to 59% post-ASCT (MRD≤10-6 45%). When evaluating based on cytogenetic risk group among patients who received quadruplet induction, MRD< 10-5 post induction was 19%, 31% and 28% (MRD≤10-6 17%, 14%, 10%) which improved to 53%, 66% and 65% respectively, post-ASCT (MRD≤10-641%, 50%, 48%) of patients with 0, 1 and 2+ HRCA, respectively.
Among patients with MRD≥10-5 post-induction, ASCT lowered the MRD burden≥1 log for 69% patients (60%, 72% and 81% of patients with 0, 1 and 2+ HRCA, respectively).
Conclusions: This dataset provides granular data to delineate the impact of ASCT on MRD as legacy consolidative strategy in NDMM and provides an important benchmark for evaluation of efficacy of TCRT as experimental consolidative strategy. This information can guide effect size calculation in the design of ongoing and future TCRT trials.