Nursing Symposium
Poster Session 2
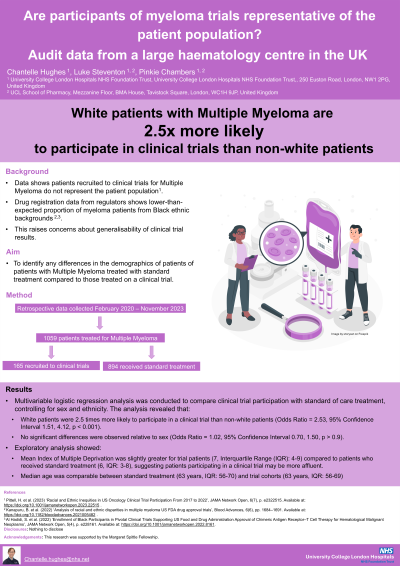
NSP-05: Are participants of myeloma trials representative of the patient population? Audit data from a large haematology centre in the UK
Thursday, September 26, 2024
Location: Exhibit Hall, Pavilion 3

Chantelle Hughes, RN, MNursSci (she/her/hers)
Senior Research Nurse
University College London Hospitals/ University College London
London, England, United Kingdom
Introduction: Multiple myeloma (MM) is a haematological malignancy characterised by clonal proliferation of plasma cells. Despite advancements in treatments, data suggests disparities in outcomes for patients diagnosed with MM relative to socioeconomic status and ethnicity. Disparities in access to clinical trials has also been demonstrated relative to these factors.
Multiple myeloma disproportionately affects people from Black ethnic backgrounds. However, patients participating in clinical trials, including those leading to approval of new therapies, are disproportionately white. This underrepresentation raises concerns about the generalisability of trial findings.
There are currently no large data sets published from the UK demonstrating trial participation of MM patients. This study aimed to assess whether patients with MM are fairly represented in clinical trials, within the context of a large research hospital in the National Health System (NHS) in England.
Methods: An audit of retrospective data from an Electronic Health Record system for MM patients treated at a single site between February 2020 & November 2023 was performed. Patients who received standard of care (SOC) treatment were compared to those treated on a clinical trial. Statistical analysis was performed with RStudio v4.3.
Results: Our dataset included 1,059 patients, of which 16% were treated in a clinical trial. Logistic regression analysis of sex and ethnicity showed white patients were 2.5 times more likely to participate in a clinical trial than non-white patients (p< 0.001). No significant differences were observed relative to sex (odds ratio=1.02, p=0.92). Median age was comparable between SOC (63 years, IQR: 56-70) and trial cohorts (63 years, IQR: 56-69). Index of Multiple Deprivation was slightly greater for trial patients (7, IQR: 4-9) compared to SOC patients (6, IQR: 3-8), suggesting patients participating in a clinical trial may be more affluent.
Conclusions: Findings support existing literature that patients recruited to MM clinical trials may not be reflective of the patient population. The observation of these issues for patients treated within the NHS demonstrates this issue may persist in countries with free access to healthcare. Underrepresentation in clinical trials is a concern as it may lead to results that are not generalisable to the broader patient population, ultimately compromising patient safety and outcomes.
Multiple myeloma disproportionately affects people from Black ethnic backgrounds. However, patients participating in clinical trials, including those leading to approval of new therapies, are disproportionately white. This underrepresentation raises concerns about the generalisability of trial findings.
There are currently no large data sets published from the UK demonstrating trial participation of MM patients. This study aimed to assess whether patients with MM are fairly represented in clinical trials, within the context of a large research hospital in the National Health System (NHS) in England.
Methods: An audit of retrospective data from an Electronic Health Record system for MM patients treated at a single site between February 2020 & November 2023 was performed. Patients who received standard of care (SOC) treatment were compared to those treated on a clinical trial. Statistical analysis was performed with RStudio v4.3.
Results: Our dataset included 1,059 patients, of which 16% were treated in a clinical trial. Logistic regression analysis of sex and ethnicity showed white patients were 2.5 times more likely to participate in a clinical trial than non-white patients (p< 0.001). No significant differences were observed relative to sex (odds ratio=1.02, p=0.92). Median age was comparable between SOC (63 years, IQR: 56-70) and trial cohorts (63 years, IQR: 56-69). Index of Multiple Deprivation was slightly greater for trial patients (7, IQR: 4-9) compared to SOC patients (6, IQR: 3-8), suggesting patients participating in a clinical trial may be more affluent.
Conclusions: Findings support existing literature that patients recruited to MM clinical trials may not be reflective of the patient population. The observation of these issues for patients treated within the NHS demonstrates this issue may persist in countries with free access to healthcare. Underrepresentation in clinical trials is a concern as it may lead to results that are not generalisable to the broader patient population, ultimately compromising patient safety and outcomes.